What are the biggest risk factors for pancreatic cancer?
Update 6 July 2023: I am still showing no evidence of active, cancer-related disease.
From what I have learned since I first suspected…this is from a layman’s experience.
The biggest factor is sheer bad luck. My surgeon (who has specialized in abdominal cancers for the better part of 30 years) said 65% of pancreatic cancer cases are basically rolling snake eyes in the cosmic craps game.
The next biggest is lousy lifestyle decisions, which I had: smoking (3 packs a day for over 20 years in my case), drinking heavily (bottle of whiskey or vodka every day for over 16 years), being overweight and underactive (check)…about 25% of cases per my surgeon.
Genetic predisposition accounts for the other 10%, which I also have from my mom’s side.
I have lost 3 close family members to pancreatic: my maternal grandmother, maternal uncle, and maternal 1st cousin. The last one, Kevin, had none of the lifestyle risk factors, and I did not.

GENERAL
- Age (close to 90 percent of all pancreatic cancers are found in people age 55 and older)
- Gender: For an unknown reason, men are somewhat more likely to develop pancreatic cancer than are women.
- Obesity
- Diabetes
- Chronic pancreatitis
- Cirrhosis of the liver
- Helicobacter pylori (H. pylori) infection
LIFESTYLE
- Smoking cigarettes: Almost a third (20-30 percent) of all pancreatic cancers are linked to smoking cigarettes. Carcinogens (cancer-causing chemicals) found in tobacco products may damage the pancreas, and smoking may add to the risks associated with other conditions, like long-term inflammation of the pancreas (chronic pancreatitis). Likewise, the risk of diabetes and obesity may also be greater if an individual smokes.
GENETIC
About 10 percent of pancreatic cancers are thought to be related to genetic factors, meaning an inherited gene mutation is passed on from parents to their children. Although these genetic conditions do not directly cause pancreatic cancer, they may increase your risks for developing the disease.
The following genetic mutations are considered risk factors for pancreatic cancer:
- Mutations in the gene BRCA2 (hereditary breast and ovarian cancer syndrome)
- Mutations in the gene p16 (familial melanoma)
- Mutations in the gene PRSS1 (familial pancreatitis)
- Mutations in the gene NF1 (neurofibromatosis, type 1)
Other inherited syndromes that may be linked to pancreatic cancer include:
- Lynch Syndrome
- Peutz-Jeghers Syndrome (PJS)
- Von Hippel-Lindau Syndrome (VHL)
- MEN1 (multiple endocrine neoplasia type 1) syndrome: A rare genetic disorder that may be a risk factor for malignant islet cell tumors.
Why is pancreatic cancer so deadly?
Update 15 DEC 2023: I am now 8 years post-chemo. Still Clear
Update 24 June 2023: I am now 8 years and 22 days post-Whipple with no signs of recurrence.
Update 2 JUNE 2020: I am now 5 years post-Whipple with no signs of recurrence or metastasis.
To echo the other respondents, pancreatic rarely evinces symptoms of its own until it is in a late stage, usually metastatic.
I am an anomaly, having been diagnosed with Stage 1B (T2 N0 M0).
The symptoms I had pointed to liver trouble or gallstones. I did not have the level of pain described by other folks in the survivor’s group to which I subscribe.
SEE ALSO |April 2024’s Leo Monthly Horoscope indicates successful outcomes.
My 1st appointment was on 23 March 2015… blood work, X-rays, ultrasounds, CT scans, ERCPs (enhanced endoscopy that placed stents in my bile ducts to relieve jaundice), and biopsies later, I received the diagnosis on 14 May.
I underwent an 8 1/2 hour pylorus-preserving Whipple procedure on 2 June. I received the pathology report on 10 June, a couple hours before I was released to home (I responded well and bounced back relatively quickly). The tumor had grown to Stage 2B (T3 NX M0).
The tumor was pretty well defined and had not invaded any other tissue. 4 of the 29 lymph nodes and 1 nerve harvested showed as suspicious, but not confirmed. I did have an adenocarcinoma. The surgeon also told me the gallbladder was in bad enough condition it would have had to come out anyway.
He also quizzed me about any past pain as the pancreas looked scarred as if I had had pancreatitis, to which I responded in the negative.
I underwent chemo from mid-July to mid-December, which I tolerated well with few side effects.
I am the 3rd of 4 cases in my family: maternal grandmother, maternal uncle, and a maternal 1st cousin.
All three of them were diagnosed with Stage 4, inoperable. My grandmother survived 5 months (1990), my uncle 19 days (2008), and my cousin 9 months (2016 – 2017). One can surmise I have genetic factors.
Edit 18 DEC 2023: I did have extensive genetic testing from a sample taken in November 2019. 87 of 88 markers showed No Significance for cancer formation.
The outlier showed Uncertain Significance for endocrine tumor formation. Mine was an Exocrine tumor.
I have a lot of bad “lifestyle” choices to look at, too. I smoked 3 packs a day for over 20 years, quitting about 20 years ago. I drank a bottle of whiskey a day for the 16 years before that 1st visit to the doctor.
I have been overweight and underactive for the better part of the past 20 years.
I may still die from pancreatic cancer, as it is an aggressive, persistent disease mechanism. If not, I will surely die with it, however many years I have left.
As of this writing (last lab work was 9 November 2017) I am showing no evidence of disease.
SEE ALSO |Are Malaika Arora and Arjun Kapoor still together?
What are the earliest signs of pancreatic cancer that should not be ignored to increase the chance of survival?
I had jaundice, moderate abdominal pain, mild fevers, and what I call “liver cramps.” All of this led me to believe I was developing liver disease or was having a blockage due to gallstones.
I underwent blood tests, x-rays, CT scans, and ERCPs with needle biopsies. All in all, it took almost 8 weeks to narrow down the actual culprit, a tumor in the head of my pancreas, which was pressing against the bile ducts.
If the stents placed during the 1st ERCP had not occluded, I would not have had the 2nd biopsy, which was conclusive. (Edit: the 1st ERCP was on 24 April; the stents worked for a couple of weeks, and then I was back in the hospital on 10 May. The 1st needle biopsy was inconclusive.
the one in May was conclusive, and the 2nd set of stents worked marvelously well.)
The main advice I have is if something feels off, get them to competent medical help and be persistent in getting an answer.
My tumor was found early enough that I qualified for a Whipple procedure without needing any chemo or radiation beforehand. There were no complications, nor any involvement of other organs, not even tendrils around a blood vessel.
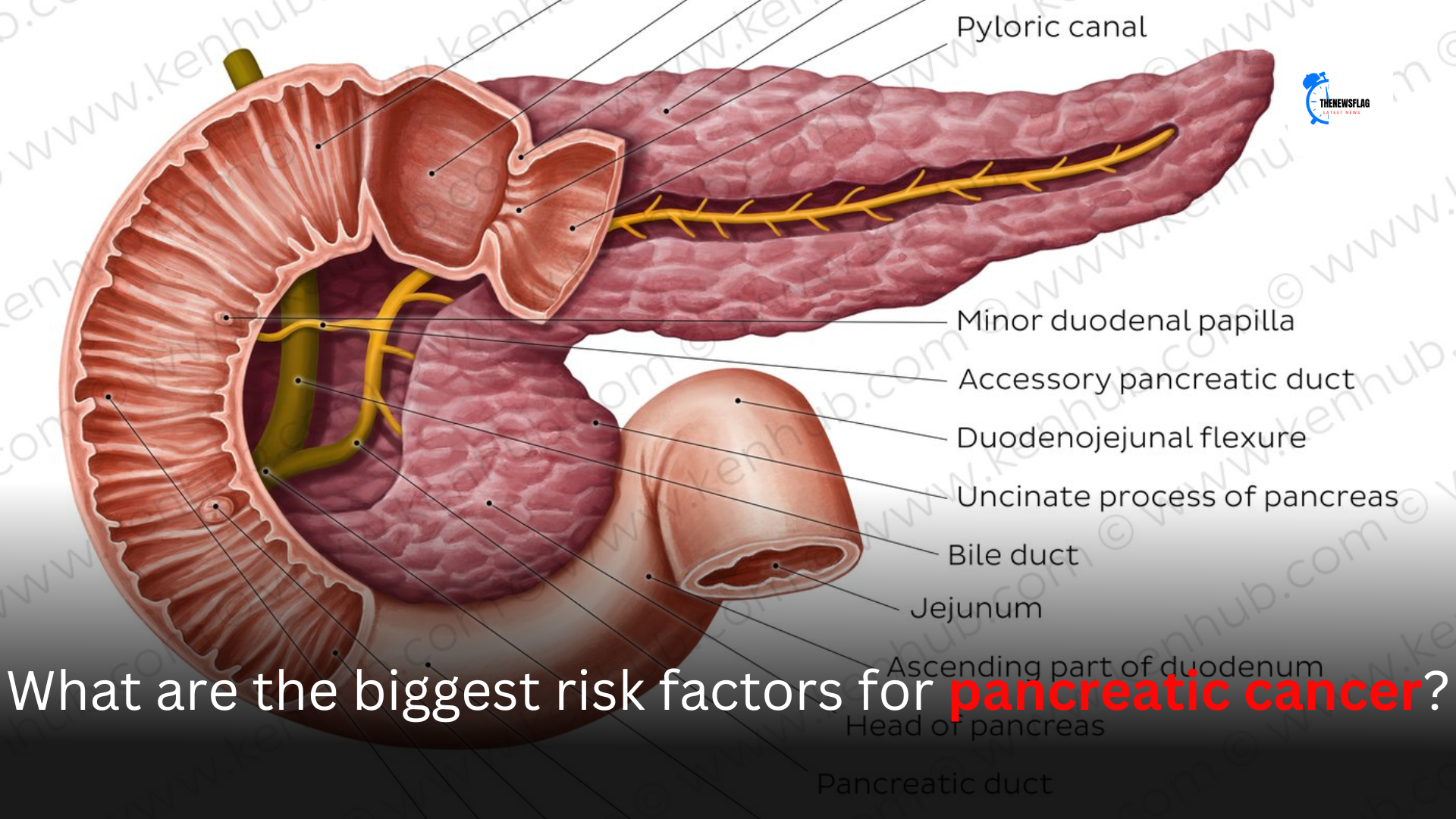
What is the function of the pancreas?
The pancreas is like a multitasking champ in the world of digestion. One of its main jobs is to produce digestive enzymes that break down the food you eat.
These enzymes, including amylase, lipase, and protease, play a crucial role in breaking down carbohydrates, fats, and proteins respectively.
But wait, there’s more! The pancreas is also responsible for producing insulin and glucagon, two hormones that help regulate your blood sugar levels.
Insulin helps your body absorb sugar from the bloodstream and store it for future energy, while glucagon does the opposite, releasing stored sugar when needed.
SEE ALSO |BGMI Maker Krafton India Launch Date: Registration Starts Now!
Now, let’s talk about the location of the pancreas. It sits snugly behind your stomach and is connected to the small intestine through a tube called the pancreatic duct.
This duct is where the digestive enzymes are transported, ready to jump into action when food arrives in the small intestine.
The pancreas truly is a team player, working hand in hand with other digestive organs like the liver and gallbladder.
When food enters the small intestine, the pancreas releases its digestive enzymes, while the liver produces bile to help break down fats. The gallbladder then stores and releases bile into the small intestine when needed.
In a nutshell, the pancreas plays a crucial role in digestion and blood sugar regulation.
It produces enzymes to break down food in the small intestine and hormones like insulin and glucagon to maintain balanced blood sugar levels. This little powerhouse is definitely an unsung hero in keeping our digestive system running smoothly!
Remember, it’s important to take care of your pancreas by maintaining a healthy lifestyle, eating a balanced diet, and avoiding excessive alcohol consumption.
If you ever have concerns about your digestive health, it’s always best to reach out to a healthcare professional for guidance.
I hope this helps you understand the amazing function of the pancreas!
What is the best way to treat the pancreas?
The best way to treat the pancreas is to eat a healthy diet and get plenty of exercise and fresh air.
The pancreas is especially influenced by diet because it has to produce insulin each and every time you eat any sugars and/or carbohydrates.
The human body can only handle about a teaspoon of blood sugar, so the pancreas releases insulin to lower the blood sugar.
So, we should give our pancreas a break by not constantly eating foods that spike our blood sugar.